Senior living needs ‘substantial and immediate financial relief’ from COVID-19, leaders tell federal government
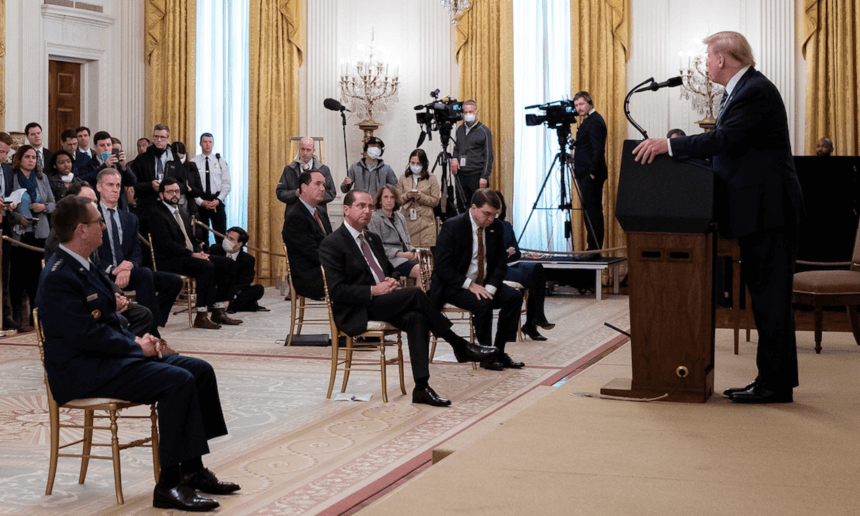
Nursing homes were the focus at an April 30 event at the White House that was attended by AHCA/NCAL CEO Mark Parkinson, Argentum CEO James Balda and LeadingAge CEO Katie Smith Sloan.
Senior living operators require “substantial and immediate financial relief” from expenses related to the COVID-19 pandemic, the leaders of four major associations representing operators of independent living, assisted living, memory care and continuing care retirement communities tell President Trump, Vice President Mike Pence, and Speaker of the House Nancy Pelosi (D-CA), with other House and Senate leaders copied, in new letters.
Congress and the administration should “prioritize the needs of the senior living industry, residents and front-line staff in the next federal legislative response package,” Argentum President and CEO James Balda, LeadingAge President and CEO Katie Smith Sloan, National Center for Assisted Living Executive Director Scott Tittle, and American Seniors Housing Association President David Schless wrote in letters dated Thursday and Friday and shared with the media on Monday.
“Senior living operators are proud to be playing a critical role in helping to ‘flatten the curve’ and avoid further burdening our nation’s hospitals during this crisis,” they said. “However, these extraordinary efforts are leading to significant financial stress, largely due to enhanced infection control measures, acquiring personal protective equipment (PPE) and related supplies, COVID-19 testing, additional staffing and incentives, and loss of revenue associated with halting new residents moving into the communities.”
Members of Congress returned to work Monday with a goal of working on another coronavirus-related aid package. Other than some funds to eligible state Medicaid providers, which would include a small percentage of assisted living operators, announced in June, assisted living hasn’t been allocated any federal funding to fight COVID-19.
The senior living leaders had six requests:
- Increased funding for the Public Health and Social Services Emergency Fund (Provider Relief Fund). The financial impact on the industry is expected to be $45 billion to $57 billion over 12 months, Balda, Schless, Sloan and Tittle said.
- Priority access to PPE, such as masks, gowns and gloves, for senior living communities. “Many parts of the country have not had full access to meet all of their PPE needs,” they wrote. “The impending second wave will bring an even greater shortage, placing residents and staff at risk.”
- Access to and reimbursement for diagnostic and non-diagnostic testing of employees and residents. “While diagnostic testing costs may be covered by Medicare for residents and private insurance for employees, recurring non diagnostic testing conducted to screen employees and residents is not covered,” the leaders said. “These costs are simply unsustainable, especially when testing residents and staff with any meaningful frequency are required under federal guidelines.”
- Priority access to the vaccine, when one is ready.
- Small business loans through Paycheck Protection Program expansion. “The program is currently limited to businesses that employ less than 500 employees, with exceptions that allow that limit to be applied on a per-location basis for businesses that are assigned a North American Industry Classification System code beginning with 72,” they wrote. “We urge similar treatment for senior living by authorizing a waiver of the affiliation rules for NAIC codes beginning with 62, Health Care and Social Assistance. This exemption should also include coverage of senior independent living communities, classified under codes beginning with 52, specifically 531110 and 531311.”
- Inclusion of all senior living employees in “hero pay” proposals that would provide an additional $13 per hour wage increase and recruitment incentives to attract insecure the workforce.
“[O]ur communities and the millions of seniors under our care must be prioritized to ensure that senior living remains a viable option for the foreseeable future,” Balda, Scless, Sloan and Tittle said, calling COVID-19-related costs “unsustainable.”
AHCA / NCAL makes additional requests
In separate action on Monday, the American Health Care Association / NCAL shared the results of public opinion research the organizations conducted among 600 women voters aged 35 to 64 to better understand their views about government support for long-term care facilities.
The research, AHCA / NCAL said, found that:
- 62% said they believed that the government did not make long-term care facilities a top priority and, as a result, did not help protect the health and lives of older adults.
- 71% said that long term care facilities need more support from the government so they can save lives and take care of loved ones.
Echoing some of the priorities enumerated in the letters to the federal government, AHCA / NCAL also made several requests of Congress for the next round of stimulus funding, among them:
- Create a $5 billion fund to which assisted living communities, skilled nursing facilities and labs can apply to cover the cost of any testing ordered by a government entity,
- Ensure that assisted living and skilled nursing facility residents and staff members are “the first and highest priority for vaccine distribution since they are the most vulnerable and at risk” for COVID-19.
- Provide access to funding for small, independent special needs plans (I-SNPs) focused on assisted living and nursing home residents to offset losses associated with COVID-19.
- Protect Medicaid.
- Offer limited immunity from liability for COVID-related activities. “This is an unprecedented public health crisis, and caregivers are doing everything they can with limited resources and information,” AHCA / NCAL said. “Providers or individual staff members who are following government guidance should not be held responsible for their good faith efforts during this once-in-a-generation pandemic.”
“Long term care facilities cannot fight COVID-19 alone. We urge Congress to make long term care a priority for funding, critical resources, and protections that will enable us to keep residents and staff safe,” the organizations said.
Article originally appeared on McKnight’s Senior Living here.



