SENIOR LIVING SENIOR DIGNITY: Summer 2020 Harsh Impact of Coronavirus Exposes the...
Blog
COVID-19 Is Tougher on Older Men, and Scientists May Now Know...
Too Little Vitamin D Might Raise Odds of Coronavirus Infection There’s evidence that low...
EHDOC Secures $30 Million Construction Loan for Redevelopment of Council Towers Senior...
EHDOC Secures $30 Million Construction Loan for Redevelopment of Council Towers Senior...
From our Chairman of the Board: Summer 2020 These Difficult Times Require Effective...
Online Safety Tips For Seniors More and more seniors have grown comfortable being online and...
Senior living needs ‘substantial and immediate financial relief’ from COVID-19, leaders...
Urgent Need for Food, Home Care, Employment, and Digital Health Supports are Ignored Policy...
NCOA Study: 3 Million Low-Income Older Adults Face Systemic Obstacles to Programs that Help...
Staying Safe As Your City Reopens: Friends And Neighbors May Be Resuming Their Regular...
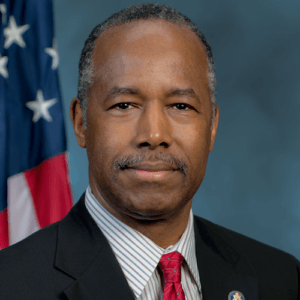
LeadingAge calls on HUD to release millions earmarked for affordable senior housing HUD...